This AI tool helps healthcare workers look after their mental health

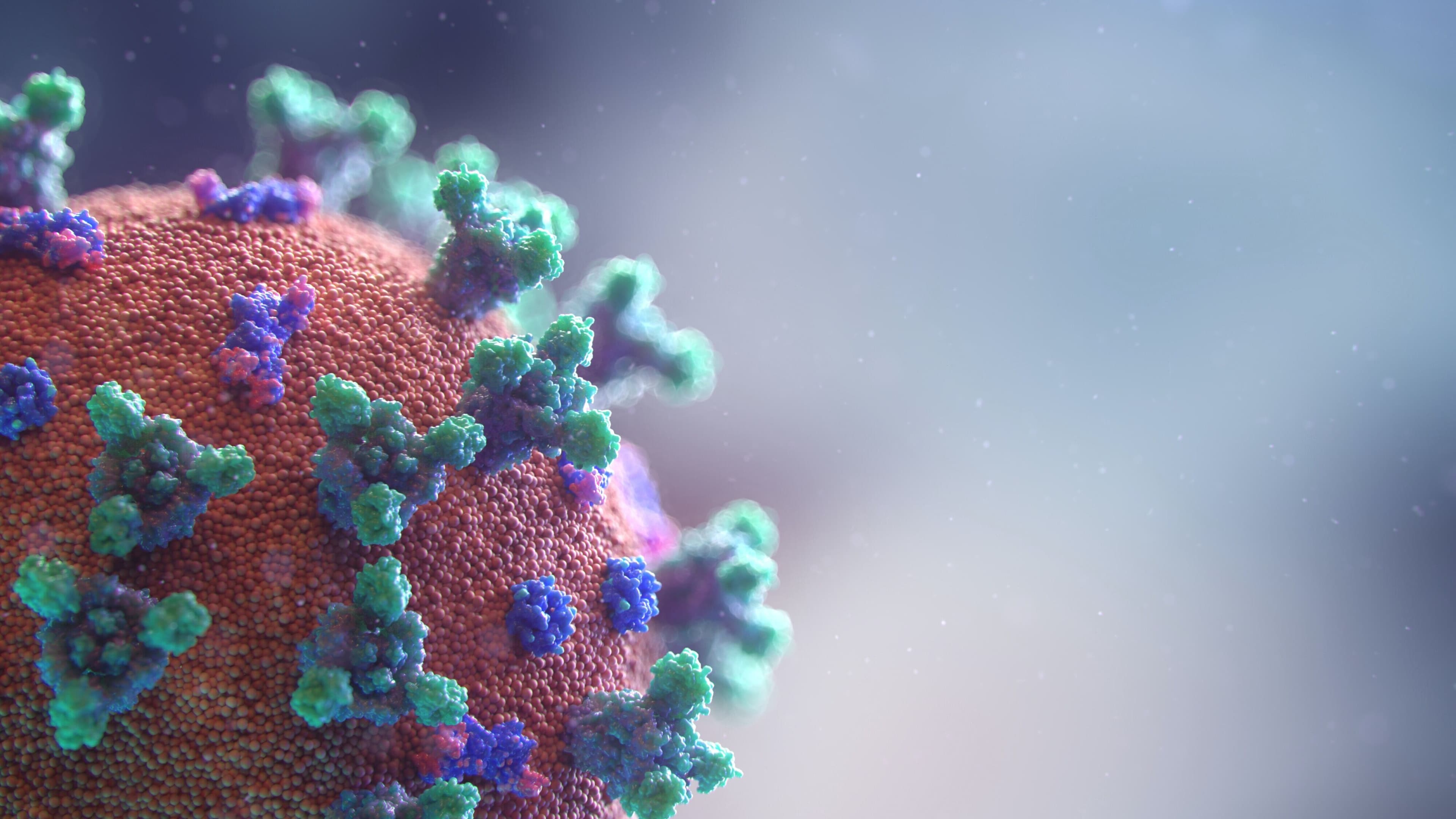
COVID-19's pressure on healthcare systems is affecting health workers' mental health around the world Image: REUTERS/Sergio Perez

Explore and monitor how COVID-19 is affecting economies, industries and global issues

Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:
COVID-19
- The pressures exerted by the pandemic mean healthcare workers are more vulnerable to developing mental health problems.
- A new AI-powered tool, developed in New York, can screen for symptoms and connect users with counselling and treatment referrals.
- It could pave the way for a wider transformation of mental health services. Here's how it works.
As the COVID-19 pandemic continues to exert pressure on global healthcare systems, frontline healthcare workers remain vulnerable to developing significant psychiatric symptoms. These effects have the potential to further cripple the healthcare workforce at a time when a second wave of the coronavirus is considered likely in the fall, and workforce shortages already pose a serious challenge.
Studies show that healthcare workers are also less likely to proactively seek mental health services due to concerns about confidentiality, privacy and barriers to accessing care. Thus, there is an obvious and pressing need for scalable tools to act as an 'early warning system' to alert healthcare workers when they are at risk of depression, anxiety or trauma symptoms and then rapidly connect them with the help they need. To address the mental health needs of the 47,000 employees and affiliated physicians in our hospital system, New York-Presbyterian (NYP) has developed an artificial intelligence (AI)-enabled digital tool that screens for symptoms, provides instant feedback, and connects participants with crisis counselling and treatment referrals.
Called START (Symptom Tracker And Resources for Treatment), this screening tool enables healthcare workers to confidentially and anonymously track changes in their mental health status. This tool is unique in that it not only provides immediate feedback to participants on the severity of their symptoms but also connects them to existing mental healthcare resources. Participants are asked every two weeks to complete a short battery of questions that assess symptoms of depression, anxiety, trauma and perceived stress, as well as potential risk factors for poor mental health and ability to function at work.
To maximise engagement, the psychiatric symptom questions in the START platform are drawn from widely validated psychiatric screening tools and adaptively selected using AI algorithms that capture the most relevant clinical symptom data in a time-efficient manner. This is achieved in two ways. First, the START platform automatically selects the most informative questions based on a participant’s previous responses in a minimum amount of time (around five to seven minutes). Second, it focuses on questions that are reliably correlated with particular functional connectivity patterns in depression-related brain networks. Much like our national airport network, brain networks are organised into a system of 'hubs' that facilitate efficient information flow, just as hub airports like O’Hare and JFK connect passengers with smaller regional destinations. Disrupted connections between brain hubs may contribute to specific symptoms and behaviours in depression.
For example, in previous work (see figure below), our group has found that psychiatric symptoms like anhedonia (a loss of interest in pleasurable activities) are reliably correlated with functional magnetic resonance imaging (fMRI) measures of connectivity in reward-related brain regions, whereas symptoms like anxiety and insomnia are correlated with differing connectivity alterations in other brain areas.

At the end of the survey, participants receive feedback on their results and are provided with options for connecting with existing and accessible mental healthcare resources. For those who need psychiatric care for their symptoms, we integrated the START platform with a telemedicine urgent counselling service at NYP that is available seven days a week and which provides faculty and staff across NYP hospitals with quick and free access to confidential and supportive virtual counselling by trained mental health professionals – a special feature of this tool and our COVID-19 response. This is important, because if treatment resources are not made immediately available and easily accessible to our healthcare workers, they may be less likely to seek help when they need it.
Within one week of deploying the symptom tracker, the utilization of our urgent counselling services had more than doubled, resulting in numerous referrals to mental health professionals. Another key element contributing to the increase in utilization was frequent communication from NYP leadership about the Symptom Tracker and the availability of crisis support. In the near future, a mobile cognitive behavioral therapy (CBT) app developed at NYP (by a group led Francis Lee) will be linked to START to target specific mood, anxiety, and trauma symptom profiles, and is currently being tested in a clinical trial for safety and efficacy.
Ultimately, we hope that such emerging digital tools will transform mental health services not only for our healthcare workers but also for larger populations affected by the pandemic.
What is the World Economic Forum doing about mental health?
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Related topics:
The Agenda Weekly
A weekly update of the most important issues driving the global agenda
You can unsubscribe at any time using the link in our emails. For more details, review our privacy policy.
More on COVID-19See all
Charlotte Edmond
January 8, 2024
Charlotte Edmond
October 11, 2023
Douglas Broom
August 8, 2023
Simon Nicholas Williams
May 9, 2023
Philip Clarke, Jack Pollard and Mara Violato
April 17, 2023